Nanoparticles in the treatment of atherosclerosis
Nanoparticles in Atherosclerosis Therapy – Real Possibilities and Limits
Pathophysiology and Therapy Targeting
Mechanisms of Nanoparticle Action
Preclinical Evidence
Limitations and Challenges
What Distinguishes Nanoparticles from “Nanobots”
Translational Perspectives
Nanoparticles in atherosclerosis therapy - real possibilities and limits
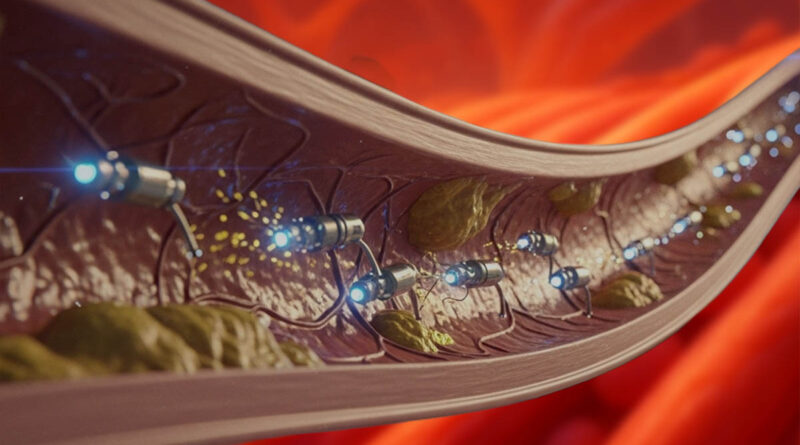
Nanoparticles are becoming one of the most promising tools in modern vascular medicine. They enable the delivery of drugs directly to sites where atherosclerotic plaque develops, avoiding high systemic doses and minimizing side effects. Their surfaces can be chemically modified to better bind to cells involved in atherosclerosis, primarily macrophages.
Additionally, many nanoparticles have a theranostic function- enabling simultaneous treatment and imaging of plaques, giving physicians the ability to monitor response to therapy in real time.
Although animal models confirm that such systems can reduce plaque volume, reduce inflammation, and stabilize their structure, the introduction of nanotherapy into the clinic faces many barriers. Biological differences, safety, long-term biodistribution, and the complex structure of human plaques mean that translation requires caution.
Pathophysiology and Therapy Targeting
Atherosclerosis is a chronic disease that develops over decades. Plaque begins to form when lipids, primarily LDL, accumulate in the vessel wall. Oxidized LDL stimulates endothelial cells, making them more permeable and proinflammatory. Monocytes, which transform into macrophages, then flood into this altered area.
By consuming oxidized lipids, macrophages become overloaded with fat and transform into foam cells. These cells produce proinflammatory cytokines, fueling a vicious cycle of inflammation. Efferocytosis, the removal of dead cells—a key process for preventing the growth of the necrotic core within the plaque- also becomes impaired.
Nanoparticles are a natural fit for therapeutic purposes in this disease because they can be designed to:
- target macrophages,
- respond to the inflammatory environment (pH, enzymes),
- modulate immune function,
- reduce oxidative stress,
- stabilize plaque by reducing inflammation and improving efferocytosis.
This approach is described in studies by Flores et al.
Mechanisms of action of nanoparticles
Nanoparticles act as intelligent drug carriers. Unlike systemic therapy, they can deliver the active substance directly to the diseased site and release it only upon reaching the plaque.
How do they work?
- Passive targeting
Atherosclerotic plaques have increased permeability and abnormal microvascular structures. Appropriately sized nanoparticles accumulate there through a mechanism similar to the EPR effect (well-known in oncology). No additional ligands are required — it arises naturally from the vessel’s physiology. - Active targeting
Nanoparticles can be equipped with ligands that recognize receptors characteristic of activated macrophages, such as SR-A1, CD36, or MARCO. This allows selective uptake and makes the treatment more precise. - Activation in the plaque microenvironment
Atherosclerotic plaques feature low pH, high enzyme activity (e.g., metalloproteinases), and oxidative stress. Nanoparticles responsive to these signals can release the drug exclusively at the disease site, minimizing side effects. - Theranostics
Systems described by NUS combine a drug with an MRI contrast agent. This means that a single nanoparticle performs both therapeutic and diagnostic roles, enabling precise monitoring of treatment effectiveness.
Preclinical evidence
Preclinical evidence includes animal models, ex vivo studies, and advanced imaging using modern techniques.
Pro-efferocytic nanoparticles (Flores et al.)
In a study published in Nature Nanotechnology, nanoparticles were developed that macrophages took up with exceptional selectivity. Enhancing efferocytosis – the clearance of dead cells – led to:
- reduction of necrotic core size,
- plaque stabilization,
- inhibition of disease progression in mice.
This represents one of the strongest pieces of evidence that targeting therapy to macrophages has profound biological significance.
pH-responsive nanoparticles, NUS (Small, press release)
The NUS team designed nanoulons that release both a drug and an MRI contrast agent in the acidic environment of the plaque.
Studies showed:
- selective accumulation in plaques,
- the ability to simultaneously treat and image,
- reduction of inflammation.
Enzyme-responsive nanoparticles (RSC Publishing)
Muñoz-Hernando et al. described nanoparticles that respond to sphingomyelinase activity – an enzyme elevated in plaques.
This mechanism enables exceptionally precise targeting because enzyme activity serves as a marker of inflammation.
Modulation of macrophage phenotype
Review articles (Chen et al.) emphasize that nanoparticles can influence macrophage phenotype, shifting it from pro-inflammatory (M1) toward anti-inflammatory (M2).
This not only reduces inflammation but also promotes plaque healing.
Limitations and Challenges
Despite dynamic development, there are real obstacles on the path to clinical therapy.
1. Differences between animal models and human atherosclerosis
Mice develop plaques faster, have more homogeneous biology, and different lipid ratios. This means that not all effects can be directly translated to humans.
2. Biodistribution and accumulation
Nanoparticles often accumulate in the reticuloendothelial system — particularly the liver and spleen.
The long-term consequences of their deposition are not yet fully understood.
3. Plaque heterogeneity
Plaques can be:
- calcified,
- fibrous,
- lipid-rich,
- actively inflamed.
Each type responds differently to therapy, making it challenging to design a single universal nanosystem.
4. Risk of destabilization
Early interventions must exclude the possibility that nanoparticles could mechanically or chemically weaken the fibrous cap of the plaque.
Detachment of a fragment could lead to embolism — therefore, safety must be thoroughly evaluated before clinical studies.
What distinguishes nanoparticles from "nanobots"
The term “nanobots” is a popular science term and does not reflect reality.
Real systems are:
- chemical, not mechanical,
- without propulsion,
- incapable of active maneuvers within a vessel,
- operating through passive and biological targeting mechanisms.
Nanoparticles are not miniature robots. Their actions stem from physics, chemistry, and biology, not from autonomous motor functions.
Translational Perspectives
The field of nanoparticle research is developing very rapidly, and many teams are working to create formulations that meet rigorous clinical standards.
What needs to happen?
- Conducting phase I/II studies to assess safety and pharmacokinetics,
- Standardization of nanoparticle production (GMP),
- Improved animal models that mimic the heterogeneity of human plaques,
- Long-term analyses of biodistribution and side effects.
Why is it worth pursuing?
Nanoparticles offer possibilities that conventional drugs cannot:
- precise therapy,
- lower doses,
- simultaneous imaging and treatment,
- targeting macrophages and inflammatory processes.
In the coming years, the first clinical studies are expected, which will answer whether the potential observed in animal models translates into real benefits for patients.
References
- Flores AM, Hosseini-Nassab N, Jarr KU, et al. Pro-efferocytic nanoparticles are specifically taken up by lesional macrophages and prevent atherosclerosis. Nat Nanotechnol. 2020;15(2):154-161. doi:10.1038/s41565-019-0619-3. PubMed record: https://pubmed.ncbi.nlm.nih.gov/31988506/
- Muñoz-Hernando M, Nogales P, Fernández-Barahona I, Ruiz-Cabello J, Bentzon JF, Herranz FS. Sphingomyelinase-responsive nanomicelles for targeting atherosclerosis. Nanoscale. 2024;16(13). doi:10.1039/D3NR06507C. Publisher record: https://pubs.rsc.org/en/content/articlehtml/2024/nr/d3nr06507c
- National University of Singapore (NUS) Yong Loo Lin School of Medicine. Researchers develop nanoparticle technology for targeted diagnosis and treatment of atherosclerosis. Press release, 18 Sep 2024. (Published in Small). NUS Medicine: https://medicine.nus.edu.sg/news/nus-medicine-researchers-develop-breakthrough-nanoparticle-technology-for-targeted-diagnosis-and-treatment-of-atherosclerosis/
- Stanford Medicine. Nanotherapy reduces plaque buildup in mouse arteries. Press release, 27 Jan 2020. (Leeper et al. nanoparticle study). Stanford Medicine: https://med.stanford.edu/news/all-news/2020/01/nanotherapy-reduces-plaque-buildup-in-mouse-arteries.html
- Chen W, Tao Y, et al. Macrophage-targeted nanomedicine for the diagnosis and treatment of atherosclerosis. Theranostics (Review, PMC open access). 2021. PMC record: https://pmc.ncbi.nlm.nih.gov/articles/PMC8580169/